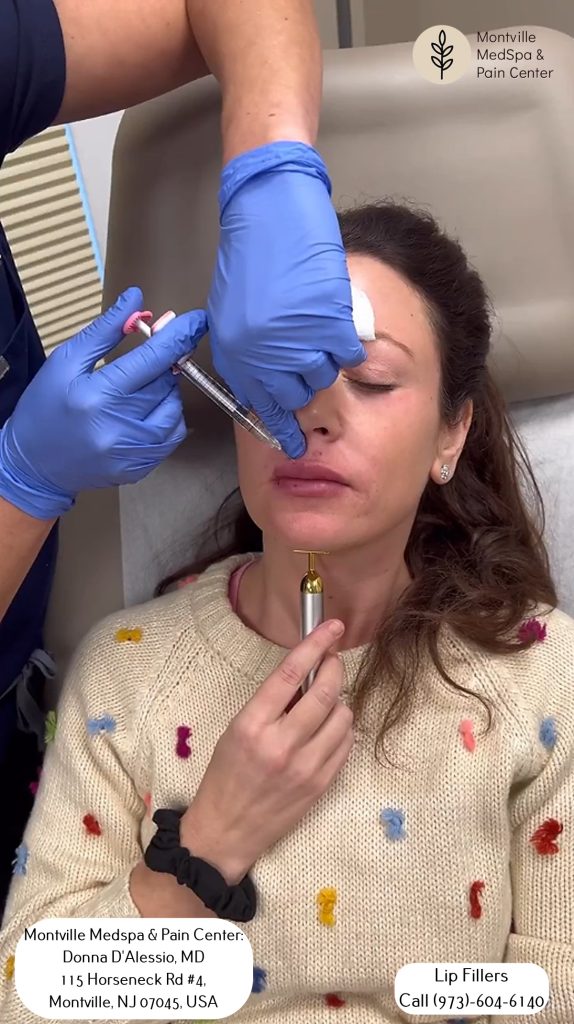
Discover the hidden dangers of lip fillers and how to avoid devastating complications, including necrosis and scarring, by being informed.
What is Vascular Occlusion?

Vascular occlusion is a severe complication that can occur during lip filler treatments. It happens when the filler material blocks a blood vessel, cutting off blood supply to the skin and underlying tissues.
If left untreated, vascular occlusion can lead to necrosis (tissue death), scarring, and permanent damage to the lips. It is essential to recognize the signs and symptoms of vascular occlusion, which may include pain, skin blanching, and swelling.
To reduce the risk of vascular occlusion, it is crucial to:
- Choose a qualified practitioner with expertise in lip anatomy and filler injections.
- Understand lip anatomy to ensure the filler is injected safely and correctly.
- Follow post-treatment care instructions carefully to prevent complications.
Educating yourself on vascular occlusion will empower you to make informed decisions about your lip filler treatments and take necessary precautions to prevent severe complications.
Understanding Vascular Occlusion
When you undergo lip filler treatments, you’re at risk of vascular occlusion, a complication that occurs when a blood vessel is blocked by the filler or compressed, leading to compromised blood flow and potential tissue damage.
Why is Vascular Occlusion a Concern in Lip Fillers?
The lips have a dense network of blood vessels, making them more susceptible to vascular occlusion. This complication is a major concern because it can lead to severe consequences if not addressed promptly.
Recognizing the Signs of Vascular Occlusion
If you experience any of the following symptoms after a lip filler treatment, seek immediate medical attention: intense pain, skin blanching, texture changes, abnormal swelling, and even potential necrosis.
Importance of Prompt Diagnosis and Treatment
Vascular occlusion requires prompt diagnosis and treatment by medical professionals to restore blood flow and prevent further complications. Understanding vascular occlusion and its risks will empower you to make informed decisions about your lip filler treatments and take proactive steps to minimize this significant risk.
Risks of Lip Filler Injections
Lip filler injections carry the risk of vascular occlusion, a serious complication that can have devastating consequences if not addressed promptly. Vascular occlusion occurs when the filler blocks blood flow, putting your lip health at risk. If left untreated, it can result in necrosis, scarring, and even permanent lip disfigurement.
Why Lips Are Vulnerable
Lips have a dense network of blood vessels, making them particularly vulnerable to vascular occlusion. This is why it’s crucial to recognize the warning signs and seek immediate medical attention if you experience any unusual symptoms.
Understanding Vascular Occlusion During Lip Filler Injections

Several factors can contribute to vascular occlusion during lip filler injections.
Inadvertent injection into a blood vessel is one cause, where filler material is injected directly into a blood vessel, blocking blood flow. This can occur when the injector mistakenly targets a blood vessel instead of the intended lip tissue.
Arterial spasm from cannula trauma is another cause of vascular occlusion. When a cannula injures the blood vessel wall, it can cause the vessel to constrict and block blood flow. This injury can occur due to the cannula’s movement or insertion.
Other complications can also lead to vascular occlusion. These include poor injection technique, inadequate training, or equipment failure. For instance, if an injector lacks proper training, they may not use the correct injection angle or amount of pressure, increasing the risk of vascular occlusion.
Even experienced injectors can encounter vascular occlusion, highlighting the importance of vigilance during lip filler procedures.
Using cannulas instead of needles can help reduce the risk of vascular occlusion, as cannulas are designed to reduce the risk of vessel injury.
Recognizing Vascular Occlusion During Lip Filler Procedures
Prompt recognition of vascular occlusion is crucial in preventing severe consequences during lip filler procedures. As a practitioner, it’s essential to be aware of the signs of vascular occlusion to take immediate action.
Signs of Vascular Occlusion
Blanched or dusky skin discoloration indicates reduced blood flow, which can be a sign of vascular occlusion. A change in skin color can occur due to reduced blood flow, and it’s essential to monitor skin tone during the procedure.
A slow capillary refill (>2 seconds) indicates arterial occlusion. A capillary refill test can help assess blood movement through tissues.
Pain during or after the procedure can be a sign of vascular occlusion. Patients may experience discomfort or pain due to reduced blood flow.
Blisters or erythema can indicate tissue damage due to vascular occlusion. The appearance of blisters or erythema is a warning sign that requires immediate attention.
Diagnosing Vascular Occlusion
Diagnosing vascular occlusion requires swift identification of telltale signs, such as skin blanching, pain, or abnormal swelling, to ensure prompt treatment and prevent severe complications.
Thorough Physical Examination
Diagnosing vascular occlusion involves a thorough physical examination, where your doctor will assess skin color changes, temperature variations, and firmness of the affected area. They’ll also differentiate vascular occlusion from other possible causes, such as infection, allergy, or bruising, to ensure an accurate diagnosis.
Prompt Diagnosis is Vital
Immediate suspicion and diagnosis of vascular occlusion are vital to prevent complications and ensure timely treatment. Your doctor will examine the affected area, looking for signs of skin blanching, pain, or swelling. They’ll also check for changes in skin temperature and firmness.
Treatment Options for Vascular Occlusion
After receiving a timely diagnosis of vascular occlusion, your doctor will create a customized treatment plan to restore blood flow and alleviate symptoms. The primary goal is to dissolve the filler and restore blood flow to the affected area.
The treatment plan may include:
- Hyaluronidase Injection: to dissolve the filler and restore blood flow.
- Additional Therapies: such as warm compresses and medications to manage symptoms and promote healing.
- Monitoring Progress: to ensure the occlusion is resolving effectively and adjust the treatment plan as needed.
- Invasive Procedures or Surgery: may be necessary in severe cases to address complications of vascular occlusion.
Follow-up
It’s crucial to follow up with your doctor within 12 hours after treatment to reassess the situation and adjust the treatment plan if needed.
With prompt and proper treatment, you can recover from vascular occlusion and regain healthy blood flow to the affected area.
Preventing Vascular Occlusion During Lip Filler Procedures

To minimize the risk of vascular occlusion, it’s crucial to choose a qualified and experienced medical injector who possesses the necessary skills to avoid accidental filler placement into blood vessels.
A skilled practitioner will have in-depth knowledge of proper injection techniques and anatomical structures, reducing the risk of vascular occlusion.
Recognizing Early Signs of Vascular Occlusion
During the procedure, it’s essential to be vigilant for early signs of vascular occlusion, such as intense pain, skin blanching, or abnormal swelling. If you experience any of these symptoms, alert your practitioner immediately.
It is vital to understand the risks associated with dermal fillers and their potential to cause vascular occlusion in the lips. Follow your practitioner’s aftercare advice carefully, and don’t hesitate to contact them if you notice any signs of vascular occlusion.
Lip Filler Safety Precautions
Ensuring Lip Filler Safety
To ensure a safe and successful lip filler procedure, it’s crucial to take an active role in verifying your practitioner’s qualifications and understanding the precautions they take to minimize risks.
Verify Practitioner Qualifications
Make sure your practitioner is qualified and experienced in performing lip filler injections to reduce the risk of vascular occlusion. A qualified practitioner will have the necessary skills and knowledge to perform the procedure safely and effectively.
Understand Lip Anatomy
Prioritize understanding the anatomy of the lips and surrounding blood vessels to minimize the chances of vascular occlusion during the procedure. This knowledge will help your practitioner avoid critical blood vessels and minimize the risk of complications.
Follow Post-Treatment Care Instructions
Follow post-treatment care instructions diligently to ensure a smooth and safe recovery. This includes avoiding strenuous activities and applying cold compresses to help prevent vascular occlusion.
Recognize Vascular Occlusion Symptoms
Educate yourself on the signs and symptoms of vascular occlusion, such as skin blanching, pain, and slow capillary refill. This will enable you to quickly identify and address any issues that may arise after the procedure.
Vascular Occlusion Complications
Timely Intervention is Crucial
Complications arising from vascular occlusion can lead to devastating consequences, including tissue necrosis, scarring, and permanent disfigurement. This emphasizes the importance of timely recognition and intervention.
Recognizing the Risks
When considering lip fillers, it’s essential to understand the risk of vascular occlusion and its potential impact on health and appearance. Skin discoloration, pain, or swelling are signs of vascular occlusion, and immediate medical attention is necessary if these symptoms occur.
Consequences of Delayed Treatment
Delayed treatment can lead to severe consequences, including skin necrosis and long-term aesthetic damage. In severe cases, invasive procedures or surgery may be necessary to restore blood flow and prevent further complications.
Prevention and Awareness
It’s crucial to be aware of the risk of vascular occlusion and take proactive steps to minimize it. Early detection and diagnosis are crucial to preventing severe complications. By understanding the risks and taking necessary precautions, you can ensure a safe and successful lip filler experience.
Long-Term Effects of Occlusion
Vascular occlusion from lip fillers can cause permanent damage to blood vessels and surrounding tissues, leading to devastating long-term effects.
If left untreated, the consequences can be severe and long-lasting. Untreated vascular occlusion can lead to necrosis, scarring, and potential disfigurement of the lips.
The long-term effects of vascular occlusion include:
- Permanent damage to blood vessels and surrounding tissues compromises blood flow and skin health in the affected area.
- Necrosis, scarring, and potential disfigurement of the lips result from permanent damage to the lip tissue.
- Scar tissue and altered lip texture form, making it difficult to correct even with surgical intervention.
- Compromised blood flow and skin health increase the risk of future complications and decrease overall lip health.
Timely treatment and proper management are crucial to prevent these long-term effects and ensure lip health.











